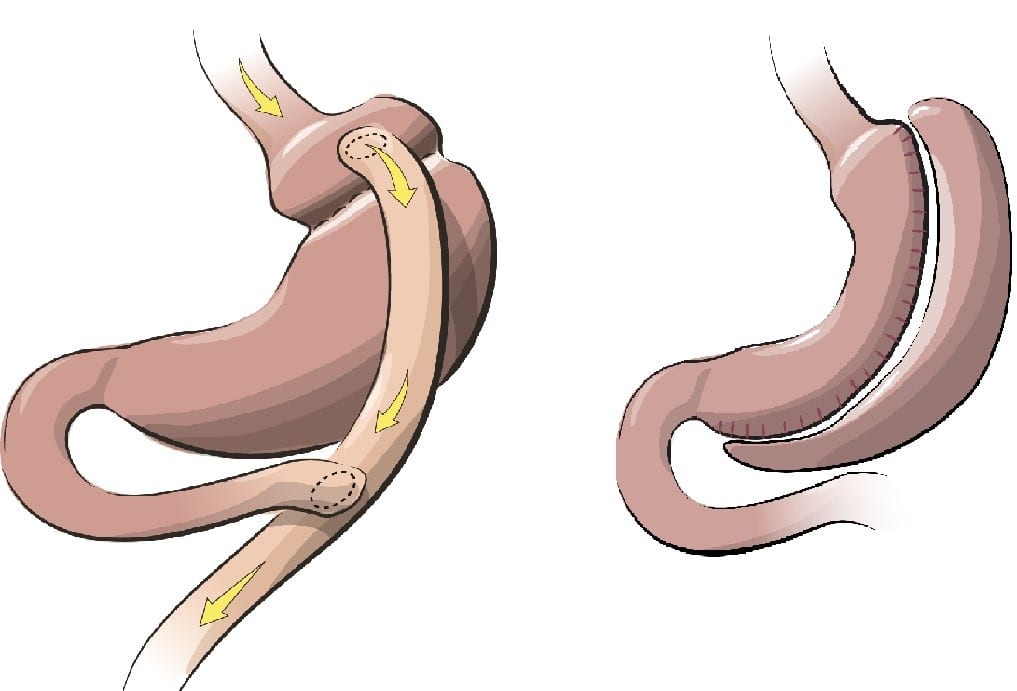
When patients are obese, it can be very difficult to lose weight, particularly enough weight to dramatically change a health condition. Bariatric surgery includes a variety of procedures to help obese patients lose dramatic amounts of weight. In the various bariatric surgeries performed by Dr. Jeffrey S Fronza, changes are made to the patient’s stomach or small intestine, or both. Patients are seen at the Bariatric clinic at Central DuPage Hospital.
A variety of long-term studies have shown these procedures to be effective for creating significant long-term weight loss, recovery from diabetes, improvement in cardiovascular risk factors, and a extending life.
Dr. Jeffrey S. Fronza performs laparoscopic roux-en-y gastric bypass and laparoscopic sleeve gastrectomy surgery. Her believes weight-loss surgery must be tailored to the patient’s needs and desires with the surgeon’s thoughtful guidance. Patients interested in bariatric surgery are seen in consultation at the Bariatric Clinic at Central DuPage Hospital.
Northwestern Medicine Central DuPage Hospital is part of a MBSAQIP accredited center of excellence. It has a proven track record of caring for the bariatric patient through the preoperative, perioperative, and postoperative process. MBSAQIP data consistently demonstrates that their patients achieve superior weight loss compared to patients cared for at other accredited centers and cared for by other surgeons.

Dr. Fronza performs all his bariatric procedures at Northwestern Medicine Central DuPage Hospital. All patients are evaluated in a multidisciplinary fashion in partnership with the Northwestern Medicine Bariatric Surgery and Metabolic Health Program.
Requirements:
Prior to your consultation, you should determine if you are eligible for surgery and if your insurance covers bariatric surgery.
- You must have a body mass index of 40 or higher to be eligible for surgery.
- If you have a body mass index between 35 and 39 and you have at least one medical problem that is made worse by obesity, then you may be eligible.
- Verify that weight loss surgery is a "covered benefit" by your policy.
- Verify that Northwestern Memorial Hospital is a part of your coverage (please note: if your insurance does not cover surgery, a self-pay option may be available).
Please contact the office to schedule an initial consultation to discuss the life-changing possibilities of weight-loss surgery.
Bariatric Surgery FAQs
Patient Resources
Patient Forms
- SAGES Bariatric Surgery Patient Brochure